-
Plan Documents
Monthly Premium
You must continue to pay your Medicare Part B premium. If you have a late enrollment penalty, it will still apply.
Part C: $0, Part D: $8.80, TARGETED LIPSA
Max out of pocket
$9,250
Medical Deductible
$257 Part B
$0
Copays (PCP/Specialist)
$0 or 20%**
Dental
$0 preventive - 2 cleanings, 2 exams, 2 fluoride treatments & a set of bite-wing x-rays per year. Full mouth x-rays are covered once every 5 years. $0 copay, no deductible, maximum benefit of $2000 per calendar year. Comprehensive dental covered 100%. Implants & dentures are not covered. PPO only network.
Over-the-counter (OTC) benefit
Flex card available
Vision
$0 routine exam. $300 yearly allowance for eyeglasses or contact lenses. 20% discount over $300 base allowance for frames, lenses, lens options. 40% discount applies on the purchase of any additional eyeglasses; must use EyeMed provider.
Hearing / Hearing Aids
$0 routine exam. $1,000 hearing aid allowance for hearing aids
Inpatient Hospital
You do not pay anything for services listed, as long as you are eligible for cost-sharing assistance under Medicaid.
$2,185 per stay max copay for unlimited days
Preventive Care
No copay for services considered preventive.
Outpatient Diagnostic Labs, Procedures, Tests
You do not pay anything for services listed, as long as you are eligible for cost-sharing assistance under Medicaid.
$0 or 20%**
Emergency Room / Urgent Care
$115/$40; worldwide coverage
Physical, Occupational and Speech Therapy
You do not pay anything for services listed, as long as you are eligible for cost-sharing assistance under Medicaid.
$0 or 20%**
Flex Card
$158 per month with rollover for retail OTC, healthy food/produce***, home modifications, pest control, utilities & fuel at the pump or rideshare services; includes retail over-the-counter
Transportation
36 one-way trips
* You must continue to pay your Medicare Part B premium. If you have a late enrollment penalty, it will still apply.
**Depending on your level of Medicaid eligibility, you may not be responsible for the copayments, coinsurance or deductibles for these listed services.
***This benefit is a special supplemental benefit for the chronically ill (SSBCI) and is made available to members with one or more qualifying chronic conditions. Not all members will qualify for this benefit. Qualifying chronic conditions include but are not limited to diabetes, cardiovascular disorders, chronic lung disorders, cancer, and dementia. For a complete list of qualifying chronic conditions please see the plan’s Evidence of Coverage (EOC).
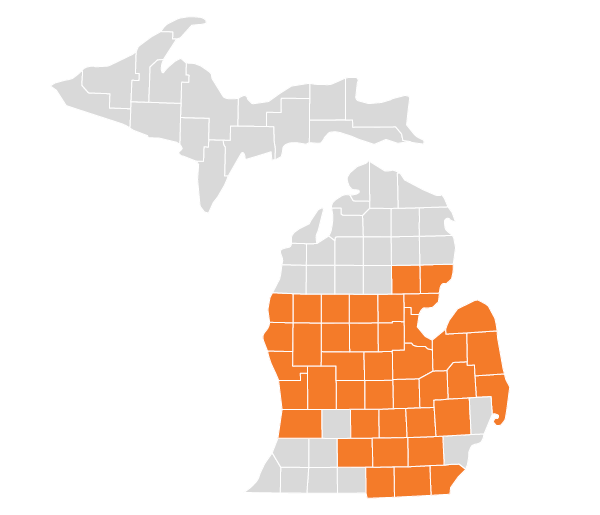
Health Alliance Plan (HAP) has HMO, HMO C-SNP, HMO-POS, and PPO plans with Medicare contracts. HAP Medicare Complete Duals (HMO D-SNP), HAP Medicare Complete Assist (PPO D-SNP), and HAP CareSourceTM MI Coordinated Health (HMO D-SNP) are Medicare health plans with a Medicare contract and a contract with the Michigan Medicaid Program that provides benefits of both programs to enrollees. Enrollment depends on contract renewals.